Eating disorders that occur early in children’s lives are associated with major structural changes in their brains, reveals a new study led by Clara Moreau, a researcher at the Azrieli Research Centre at CHU Sainte-Justine in Montreal.
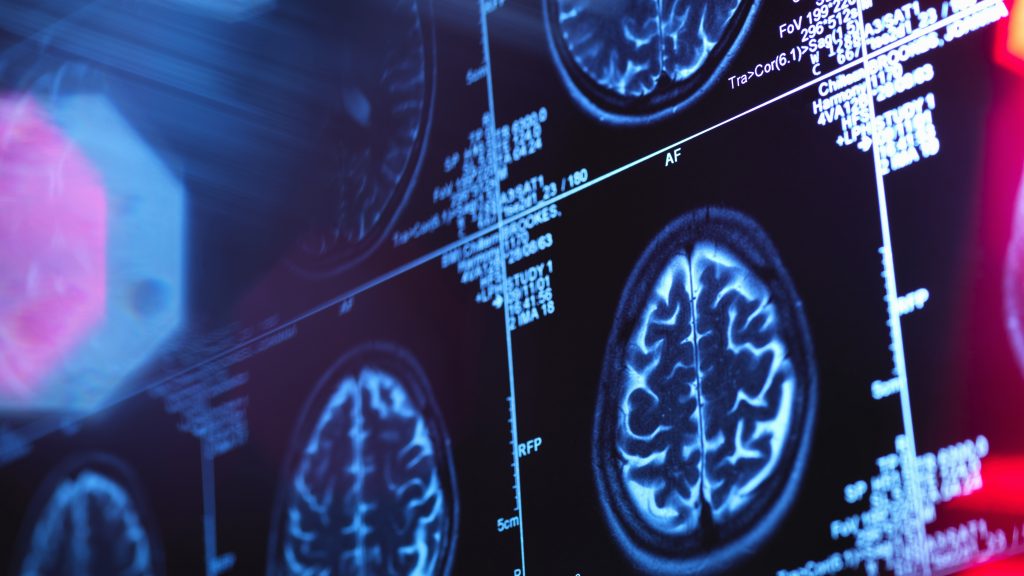
By analyzing brain images obtained by magnetic resonance imaging (MRI) of a sample of 290 children aged 7 to 13, Moreau observed in anorexic children a significant and generalized thinning of the cerebral cortex.
This phenomenon had recently been documented in adolescents and adults suffering from anorexia, she said, which suggests a significant impact on the brain, regardless of age.
Related:
“We wanted to see if anorexia was associated with anything at the brain level. Because radiologists tend to think it isn’t. And then, ultimately, we found significant alterations. When I say significant, it’s one of the strongest we find in psychiatry, stronger than in autism or schizophrenia,” the researcher marvels.
The thinning of the cerebral cortex will have an impact on the lives of young people suffering from anorexia, but this phenomenon can be reversible provided there are no too many relapses.
“In fact, the brain, the structures, they are still there, they are not destroyed, but on the other hand, all the fat is removed (the brain is made up of a lot of fat). […] The child will not necessarily have memory problems, but rather difficulties learning things quickly, concentrating,” explains Moreau, who is also an assistant professor at the Faculty of Medicine of the University of Montreal.
The child will have to work twice as long as another to learn the same thing, because his brain will be slowed down, she illustrates.
“What we see is that even if there is a large, rapid weight loss, the brain, in a young child, can recover very quickly. On the other hand, if this anorexia lasts, if it becomes chronic, and if there are several episodes, and it lasts until adulthood, then we may not have the recovery we are necessarily hoping for, because the brain has to get used to this state of continuous deficiency. And therefore, it can alter its general development,” warns Moreau.
Loss of gray matter
Clara Moreau also analyzed the impact on the brain of another eating disorder: selective or avoidant eating disorder (SED), which is better known by its English acronym ARFID (Avoidant/Restrictive Food Intake Disorder).
ARFID involves restricting food intake or eating only certain types of foods, but without any desire to lose weight and without a distorted body image. Moreau points out that this disorder usually occurs in young children and affects more boys than anorexia, where girls are more prevalent.
With her team, Moreau discovered that the thickness of the cerebral cortex remains intact in children with ARFID, but there is a decrease in intracranial volume and gray matter.
Children as young as 5 or 6 years old can be affected by ARFID. “It begins early in development, and so we think the brain adapts to this low calorie intake over the years. Basically, the child remains below the weight curve of a normal child. A child with ARFID will always be below this, so their brain development will also be below this,” explains Moreau.
The two eating disorders have very distinct effects, the researcher explains. “In anorexia, all of a sudden, the child will lose 10 kilos in three months. So, the brain will suddenly thin enormously, almost like an inflammatory reaction. Whereas in ARFID, it’s progressive, it lasts for years. We have an adaptation of the whole body that isn’t necessarily good, but in any case it’s there,” she explains.
However, the effects on the brain are difficult to reverse for ARFID, even if children gain weight. “It’s as if these volumes of gray matter are more difficult to recover,” points out Moreau. “On the other hand, children with ARFID tend to function better cognitively than those with anorexia.”
A third of patients relapse without anyone knowing why.
Moreau’s research could help provide better support for children who relapse. Approximately 35 per cent of patients at Sainte-Justine Hospital return to the hospital after an initial episode of anorexia. “Everything has been done to help them get better, they’ve gained weight, they’re on a good recovery curve, and they relapse. We have a third of patients who will relapse. We don’t currently know why these patients relapse and not the others. What differentiates them? There is no clinical trait that differentiates them that would allow us to know in advance that these patients are at risk,” the expert maintains.
Her study, recently published in the scientific journal Nature Mental Health, provides insights into these issues. Patients who have not fully recovered in terms of brain function, even if they have recovered in terms of weight, may be at greater risk of relapse.
Moreau wants to shed light on this specific aspect. She first conducted a cross-sectional study, which followed patients at a hospital in Paris, France, who were at different stages of relapse. “We were able to hypothesize that there is indeed recovery, that it’s going quite well, particularly among younger patients. But what we want to do now is confirm this, scan patients at various points in their recovery and monitor those who are going to relapse,” she explains.
Moreau is now embarking on a longitudinal study that will follow patients from the same hospital in Paris in addition to a cohort at Sainte-Justine Hospital.
—The Canadian Press’s health content is funded through a partnership with the Canadian Medical Association. Editorial choices are solely those of The Canadian Press.
–This report by La Presse Canadienne was translated by CityNews